In June of 2020 I noticed a very hard lump in my biceps area. I ignored it as I go to the gym regularly. My best friend Drew is a representative level athlete and knew it was not a sporting injury. He pushed me to call my mum. She made me immediately go to the GP.
The GP was very good and organised an immediate scan and ultrasound for the very next morning. That was a very stressful time for me. I was relieved to find out it was not Osteosarcoma or Fibrosarcoma like they were concerned about. It was put down to a muscle tear. My mother was not convinced and requested an urgent MRI the next day. The result came back as a rare 3 in a million desmoid tumour. It was very confusing. I was told I needed systemic chemotherapy and had to be seen by a Sarcoma Specialist yet it was not normal cancer. Rather a chronic sub form of sarcoma.
The sarcoma surgical team at Chris O’Brien Lifehouse were excellent. They fast tracked everything to be safe and knew not to remove the desmoid as can trigger its return with a vengeance. The necessary surgical biopsy however triggered it. Sometimes desmoids can turn off so a wait and see approach can be useful at times. It was clear mine was growing however and luckily my mother was doing extra MRIs.
Desmoids behave like sarcoma in every way apart from they rarely metastasise. They are locally aggressive and grow like a vine eating everything in their way . As they are aggressive when in the head, neck or intra abdominal areas they can be deadly. They often do not respond to chemotherapy or radiation. Just like other forms of sarcoma.
I did not want to face amputation or a lifetime on and off chemotherapy. Radiation was also being repeatedly suggested despite globally being the last treatment option due to the medium term risks of a deadly radiation induced sarcoma. I was determined to find another way as was my mother, and we were not OK with the suggested further wait and see approach when it was clearly growing.
Luckily we found out about an Israeli trial by Dr Eldad Elkanave via the wonderful support of the DTRF in America, and we switched teams. I felt a sense of relief I cannot adequately describe once I changed. Interventional Radiologist Dr Glen Schlaphoff from Spectrum Imaging/Director of Liverpool Hospital Interventional Radiology and Dr Antoinette Anazodo from Prince of Wales Children’s Hospital changed my life. They gave me hope. They both have the most outstanding patient centred approach alongside incredible medical knowledge and skill-sets in their fields. They backed my wish to have TACE (chemo-embolisation) followed by cryoablation.
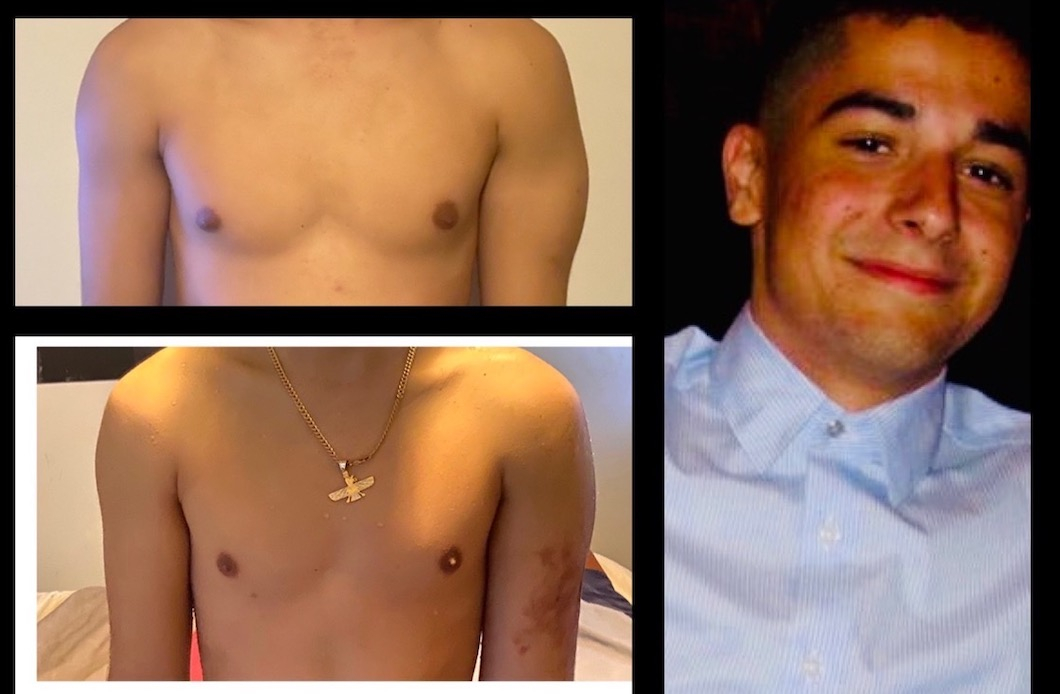
I have had five procedures to date. My tumour had grown from 5cm by 2cm by 3cm to 15cm by 9cm by 10cm before treatment started in February 2021 under my new team. Dr Elkanave was involved from Israel which I will not forget. It is now back down to 5cm by 2cm by 2cm. I am the first patient in Australia to do this and first globally to do this first line treatment for my tumour type. It has allowed me to get on with life in between treatments without the harsh cardiac, fertility, mental health and immune related side effects on systemic chemotherapy.
I would not have completed my HSC or now be at University likely without my parents, Glen and Antoinette’s determination to help change the trajectory of desmoid patient treatment outcomes. Antoniette attended every appointment – even regular check ups with my lovely burns nurse Alison. Their Oncology nurses Fiona and Cathy are the best too. Glen is my hero for the rest of my life! There may not be a lot of fancy advertising but Prince of Wales Hospital walks the talk when it comes to comprehensive Oncology care for their adolescent patients. Many others with my tumour type are now choosing the TACE and Cryoablation treatment pathway where feasible globally which makes me so happy. I would like to work with stakeholders to see Cryoablation covered by private health funds like it is in the USA and Europe.
Lastly, I know my medical journey is not over. A desmoid tumour diagnosis is a chronic condition. One must have a warrior attitude. The reality is I have many battles ahead to win the war. It is so confronting to sit next to other patients with more deadly forms of sarcoma knowing what that prognosis means. Cooper was the same age as me when diagnosed. His tumour was in the same location.
It is just not OK that Osteosarcoma and Ewing’s Sarcoma have not seen improvements in 40 years. I will help in any way to change this. Any progress with one form of sarcoma helps another form. For Cooper, for every patient I sit next to on my check up days, for all the rare desmoid patients, and future sarcoma patients I wish for nothing short of a cure ASAP and better support while we achieve that.
I want all patients to have doctors that are patient centred, have sound consultation skills, are determined by nature, and up to date with the latest clinical knowledge. Explaining ALL options available and involving patients in decision making is also key. I want patients who do not have parents who are skilled researchers to have somewhere to turn to in Australia. Be it private or public ALWAYS seek a second or third opinion if concerned and look into trials.
Always remember what extreme talent we have in our Teaching Hospitals! – Christopher Sabahi 2022