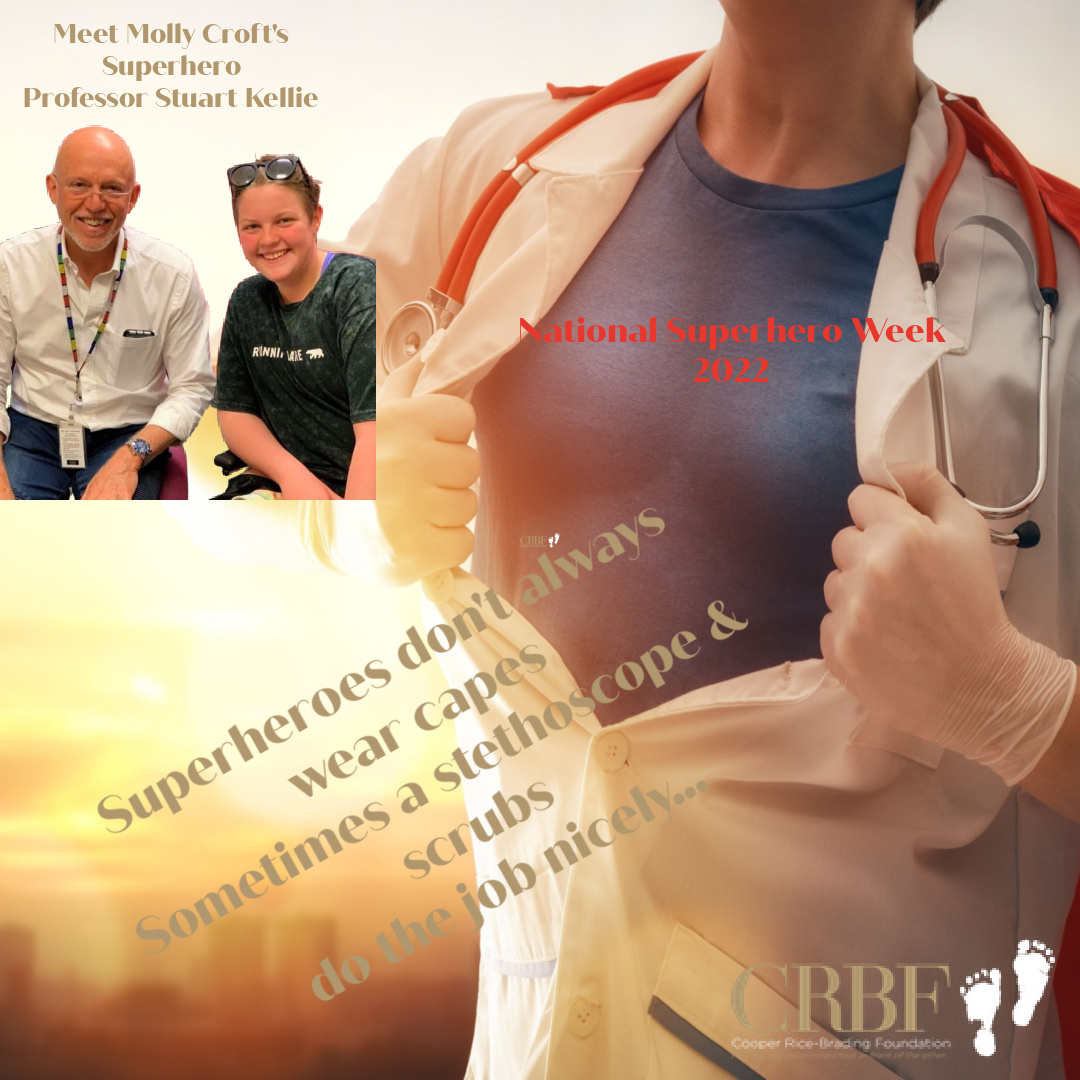
“I believe a real-life superhero is someone who has extraordinary or superhuman abilities or skills. They are people who deserve our gratitude.
During my cancer journey I could name a few, however right at the top of this list is my oncologist Professor Stewart Kellie, the best of the best in my eyes.
After being diagnosed on my 12th birthday with high grade metastatic osteoblastic osteosarcoma, I thank the universe every day for Prof Kellie being assigned to me.
He told me that over the next few months things were going to be tough, I would lose most of the bone in my leg and would have to undergo many rounds of chemotherapy to beat this disease (no different to anyone fighting this hideous disease). But he also promised me that he would always tell me the truth, he would never lie to me no matter how hard his news was. That I had to trust him always and we would get through it all together.
He kept his promise to me, he made me feel so safe and protected and I knew he had my back.
I had a lot of time to think about things while being treated. How dedicated the doctors and nurses were, wondered what their families were like, and how hard Prof Kellie must have worked to become the amazing man he was. I was grateful for him from the beginning.
After many operations and many months of chemotherapy it was also Prof Kellie who delivered the news to me that I was cancer free and I was able to go back home to my hometown, some 300km from the Sydney Children’s Hospital at Westmead.
When Prof broke this news to me, you can imagine the relief for me and those around me. In our last appointment before we left that day Prof said to me “Molly, any more questions before you go?”. I said “Yes Prof I have one. You are one of my real-life superheroes, and I’ve always wondered what superheroes eat. Prof what did you have for dinner last night?”.
We laughed, he answered my question, and I was lucky enough to go home shortly after.
When I relapsed more recently it was again my superhero Prof Kellie that delivered the news after a routine scan. I knew it upset him too, but he again had the ball rolling and I knew I was in the hands of the best.
After my surgery, where they removed the sarcoma nodules from my lung, one of the first people by my bedside on the ward was Prof Kellie.
When I spotted him I burst into tears. Prof said “I’m glad I don’t have this effect on all my patients Molly” before my Mum said “Moll why are you crying, Prof doesn’t make you sad does he?”. I responded with “No he doesn’t. He makes me feel safe and I’m so glad to see him”.
And that why he is my superhero – he is extraordinary, he is so skilful and super, super clever. Regardless of the news he has had to tell me, he has always made me feel safe and he deserves my gratitude.
So, Professor Kellie, this superheroes week for 2022, I hereby rename you – Superhero Professor Stewart Kellie.
You are my real-life superhero and I salute you. Today, always, and forever.” Molly Croft